
Overview
This outpatient procedure consists of an acidic solution applied to the skin, which removes the outermost layers of cells and allows the skin to rejuvenate.
Medium peels are commonly used to treat acne scars, fine wrinkles, blemishes, and pigmentation problems, and often work well for patients with darker complexions.

Preparation
Before the peel, facial skin is cleansed and sterilized.
Medium peels may be performed while the patient is lightly sedated, and can be used on the entire face or on selected portions of the face.

Procedure
A chemical solution is carefully applied by the dermatologist to select areas of the face, and is usually left on the skin for less than 1 hour.
The solution is then gently washed away with water, after which, a soothing ointment may be applied.

Recovery
After a medium chemical peel, the skin will be sensitive, and may be swollen and red for about a week. The outer layer of skin will then begin to flake off, revealing fresh skin beneath.
The entire process takes about two weeks. In some cases, more than one treatment may be necessary to achieve the desired result.

Overview
This nonsurgical procedure is used to treat blemishes on the skin's surface.
Ablative laser resurfacing can smooth fine wrinkles and scars, and promote the growth of healthy new skin.
Ablative laser resurfacing can have dramatic effects after just one treatment.

Preparation
Before the treatment, facial skin is cleansed and sterilized.
Anesthesia or sedation may be administered, depending on the type and extent of treatment.

Procedure
The dermatologist directs a handheld laser over the surface of the skin at the treatment area. The laser vaporizes the skin's surface, exposing the fresh new skin underneath.
Laser resurfacing can be effective for targeting fine wrinkles, blemishes, uneven pigmentation, loose skin, and burst blood vessels.

Recovery
When the procedure is complete, the dermatologist may apply a topical medication and dress the skin.
After the procedure, the skin will be red, swollen, and sensitive. The skin will scab over and heal over the next few weeks, leaving fresh new skin in its place. The entire process takes between 6 and 12 weeks.

Overview
This outpatient procedure is used to remove and examine tumors of the skin to ensure that the entire cancer is eliminated and none of the "roots" of the cancer are left behind.
The Mohs technique is often used to treat cancers of the face and neck.

why mohs?
Mohs surgery is a conservative treatment designed to leave as much healthy tissue as possible, while eliminating the cancerous cells completely.
It is often the surgery of choice for patients who have recurrent, aggressive, or unusual tumors, or for patients who have tumors in highly sensitive areas.
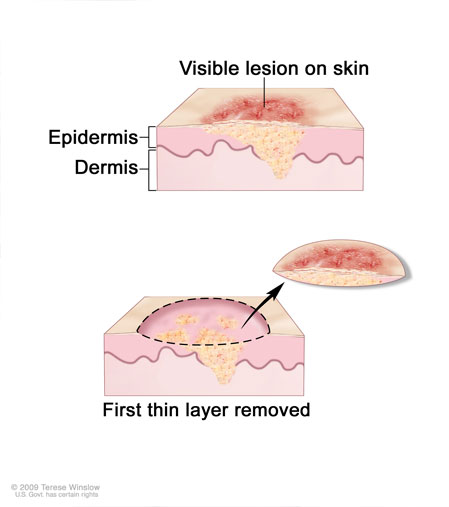
Removal
The skin is first sterilized and local anesthetic is administered. The dermatologist then carefully cuts away the section of tissue that contains the cancer.
The surgeon charts the way it was oriented in the skin so that the cancer can be accurately mapped.
Examination
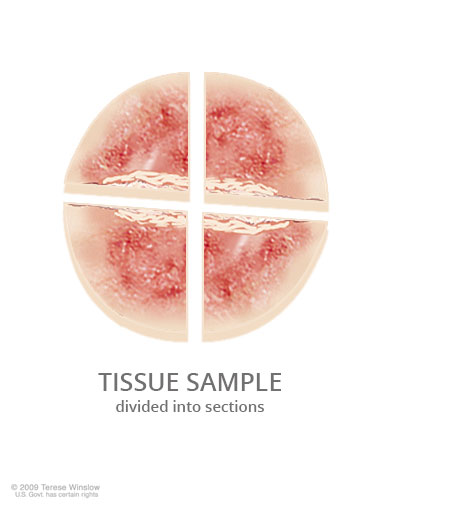
The wound is dressed, and the patient waits while the tissue sample is examined in the lab.
The tissue is divided into sections, then frozen and studied under a microscope. The dermatologist looks for any traces of cancer that extend beyond the section of skin that was removed.
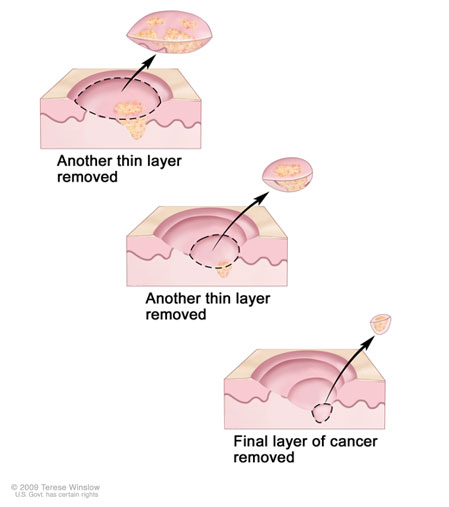
Additional Removal
If the dermatologist sees that traces of cancer may remain, the procedure is repeated until no traces are detected.
The wound is uncovered, and additional tissue is removed from the questionable area. The new sample is examined microscopically, and the process is repeated until the dermatologist is sure that all of the cancer has been removed.

End of Procedure
Once the removal is complete, the surgical site is closed.
In some cases, a plastic surgeon or reconstructive specialist may be needed to finish the procedure.
The patient is monitored during future visits.

Overview
This non-invasive, outpatient procedure uses a mild chemical solution, called a sclerosant, to treat spider veins and varicose veins.
In some cases, ultrasound may be used to guide the injection.
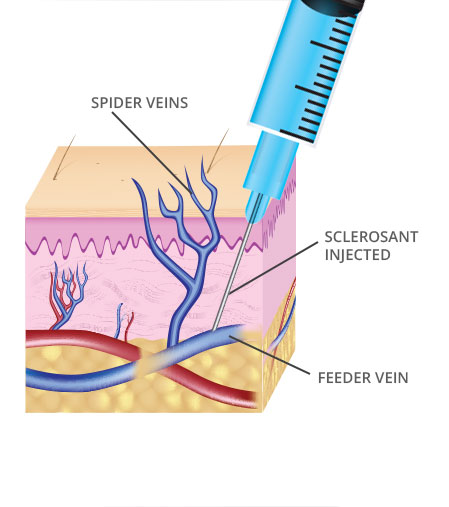
Procedure
After the area is cleansed and sterilized, the dermatologist inserts a needle into the target vein and injects the sclerosant.
In cases of spider veins, the dermatologist may treat the feeder vein, which supplies blood to the visible branches.
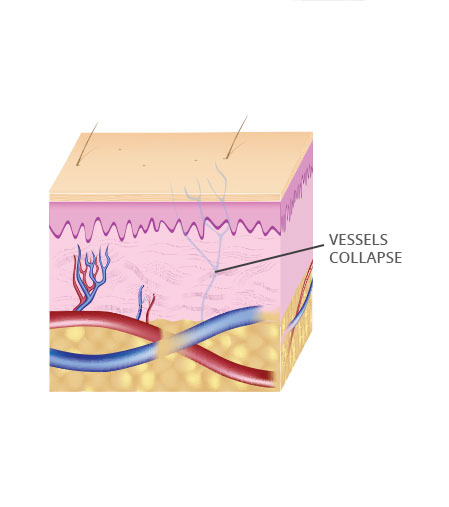
Vein Collapse
The sclerosant irritates the wall of the blood vessel, causing it to restrict and collapse. The flow of blood will be redirected to other healthy veins in the area.
The dermatologist may make multiple injections along the target vein to complete the treatment. Over time, the body will absorb the collapsed vein.

End of Procedure
The leg is bandaged tightly for several hours to help keep the treated vein closed.
Patients will be able to return to normal activities immediately after the procedure. Compression hose may need to be worn for several days after the procedure.

Overview
Acne is the formation of multiple blemishes on, or just beneath, the surface of the skin, usually on the face, neck, chest, shoulders and back.
Acne can affect anyone, but it most commonly affects adolescents and young adults.
Causes
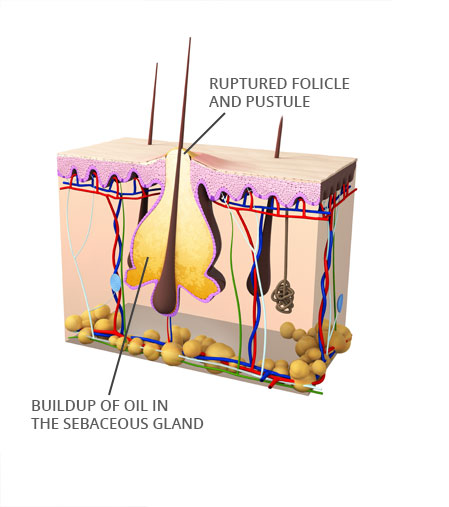
Acne occurs when small openings in the skin, called pores, become blocked with dead skin cells and oil.
A blocked pore causes a buildup of oil in the sebaceous glands. These are the oil-producing glands of the skin. When trapped oil builds up within these glands, bacteria can multiply rapidly, which causes inflammation of the surrounding tissues.

Types of Blemishes
Acne blemishes may take the form of large pustules (pimples) or small red bumps (papules).
Small, dark clogged pores (blackheads), or small, white bumps (whiteheads) may also form, as well as small nodules or cysts beneath the skin.

Triggers
Acne breakouts can be triggered by hormonal changes associated with puberty or pregnancy, certain medications, and by a diet rich in dairy or carbohydrates.
Acne is not caused by eating greasy or sugary foods or by having dirt on the skin.

Treatment
Acne is usually treated with cleansing products designed to remove excess oil and bacteria from the skin.
Acne can also be treated with prescription-strength topical or oral medications, laser or light therapy, and cosmetic procedures such as chemical peels and microdermabrasion.

Overview
Eczema, also known as dermatitis, is a general irritation and swelling of the skin.
Eczema can include several types with varying symptoms.
Causes
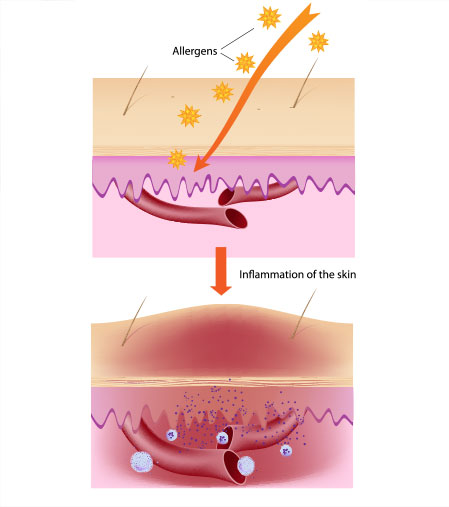
The exact cause of eczema is unknown, but may be similar to allergies where the body's immune system becomes hyperactive due to a certain trigger.
Some triggers for eczema may include exposure to rough fabrics, cleansers and soaps with harsh detergents, high and low temperatures, stress, certain pollens, and animal dander.

Symptoms
The most common symptom of eczema is red, itchy skin. The skin may appear dry and puffy around the red areas, and may feel scaly and flake off.
Eczema most commonly appears on the face, knees, hands, and feet.

Treatment
Although there is no cure for eczema, it is not life-threatening and can be managed.
Treatments include moisturizing creams, cold compresses, topical and oral corticosteroids, antihistamines, and light therapy. Avoiding soaps, detergents, or creams with scents or harsh chemicals can also help reduce occurrences.

Overview
Psoriasis is a common, and chronic skin disease that can cause dry, itchy, painful patches of skin.
Causes
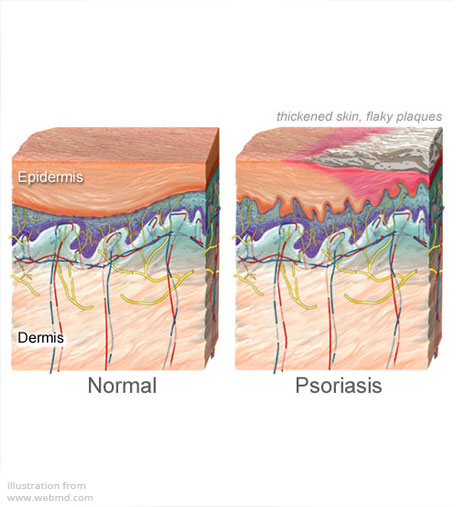
Psoriasis is caused by a malfunction in part of the immune system that results in the immune system attacking healthy skin cells.
The skin responds by over-producing replacement skin cells. These cells grow rapidly beneath the skin and then rise to the skin's surface, where they build up to form scaly patches.

Triggers
Psoriasis can be triggered by infections, stress, cold, dry weather, and changes in climate or environment. It can also be triggered by alcoholic beverages, skin irritation from allergies or scratches, and some medications.

Symptoms
The main symptom is red patches of dry, itchy skin, usually covered by flaky white or silver scales. These patches may be small, or may cover large areas of the body.
The patches may be painful, and may crack and bleed. Rough fingernails is also common. The symptoms of psoriasis may come and go throughout a person's life.

Psoriatic Arthritis
If a person who has psoriasis also experiences joint pain, stiffness and swelling, these may be signs of psoriatic arthritis, a form of debilitating arthritis that can develop gradually over time.

Treatment
Treatments include medicated creams, soaps, and shampoos. Moisturizers may prevent flaking. Avoidance of irritating cosmetics and soaps may lessen symptoms. Light therapy is also used, including exposure to sunlight.
In cases of severe psoriatic arthritis, surgery may be needed to repair or replace a damaged joint.

Overview
Rosacea is a common skin disorder that causes chronic inflammation and redness, usually around the forehead, chin, cheeks and nose.
Rosacea is often mistaken for acne or skin allergies, and most commonly occurs in adults over age 30.

Causes
The exact cause of rosacea is unknown, but a variety of factors are known to cause flares. These triggers include sun exposure, extreme weather, exercise, emotional upsets, spicy food, and alcohol.
Contrary to popular belief, alcohol does not cause rosacea - although it can cause rosacea symptoms to worsen.

Risk Factors
Rosacea most commonly affects adults between age 30 and 60, and tends to run in families. It is most common in women (particularly during menopause), but severe cases of rosacea occur most in men.
Although rosacea can develop in people of any skin color, it tends to occur most frequently in people with fair skin.

Symptoms
Rosacea can develop in people of any skin color, but occurs more more frequently in people with fair skin.
Many people with rosacea also experience eye problems, including redness, inflammation, itching, burning, or dryness. Most cases of rosacea are cyclic - symptoms may flare up or lessen for weeks at a time.

Treatment
A doctor may treat rosacea-related skin problems with topical or oral antibiotics. Rosacea-related eye problems can be treated with oral antibiotics, steroid eye drops, and good eyelid hygiene.
Although there is no cure, rosacea can be treated and controlled to improve the appearance of the skin.

Overview
Scars are the body's way of healing the skin after injury. A scar's appearance depends on the type of wound and where it is on the body, but other factors such as age, sex, ethnicity, and heredity can also play a role.
Scars may fade over time or with treatment, but they will never completely disappear.
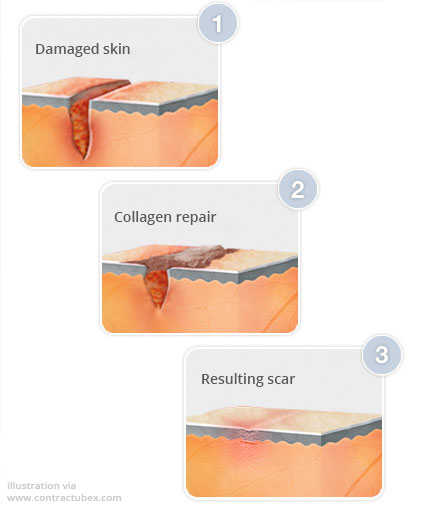
Causes
When the thick layer of skin, called the dermis, is damaged, the body repairs it with collagen, eventually forming a scar.
Scars are caused by trauma to the skin from incisions or burns, and can also be caused by conditions such as acne or chickenpox.

Appearance
Scar tissue looks different than normal skin, and typically appears flat and paler than surrounding skin. Scars can vary greatly in appearance depending on location, cause, age, and skin type.
Acne scars can form deep pits, while burn scars often have a wavy, stretched appearance. Young, and dark-skinned persons may develop raised scars.

Treatment
Treatment options depend on the type of scar, and may include topical applications, steroid or collagen injections, laser resurfacing, or surgical removal.
Scars cannot be completely removed, but treatment can help make them less noticeable.

Overview
Because moles can become cancerous, it's important to be aware of the characteristics that can signal skin cancer. Dermatologists use a handy mnemonic device to remember these characteristics: ABCDE.
With early detection and treatment, most cases of skin cancer can be cured.
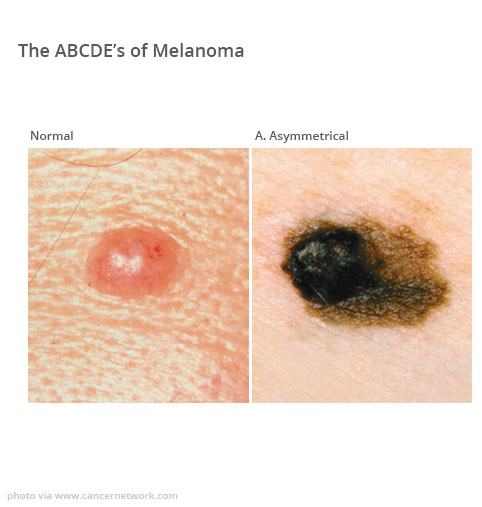
A. Asymmetry
Normal moles generally have a regular shape. If one half of a mole is unlike the other half, the mole is suspicious.
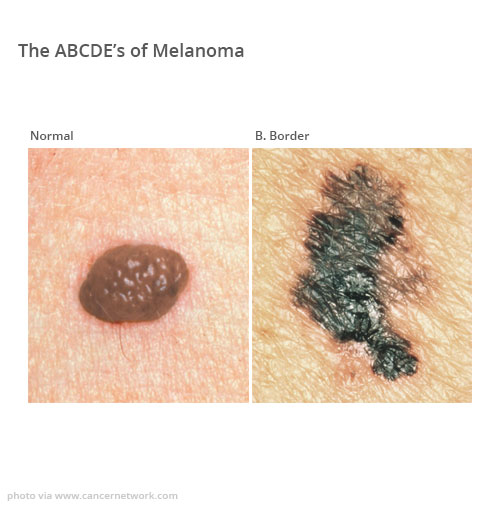
B. Border
Normal moles have smooth, even borders. Moles that have irregular, poorly defined, notched, or scalloped borders are suspicious.
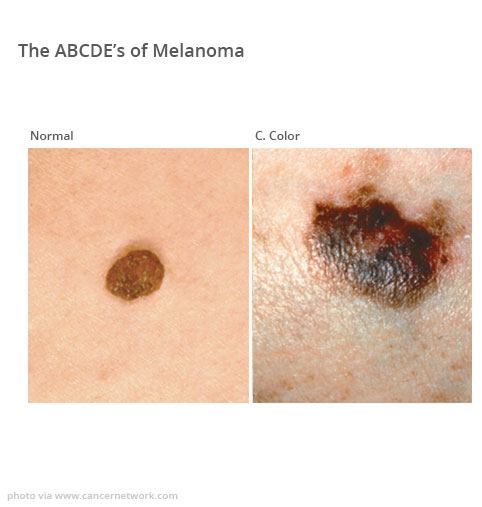
C. Color
Normal moles are a single color, usually brown or black. Moles that have different shades of color, multiple colors, or atypical colors such as white, blue, or red are suspicious.
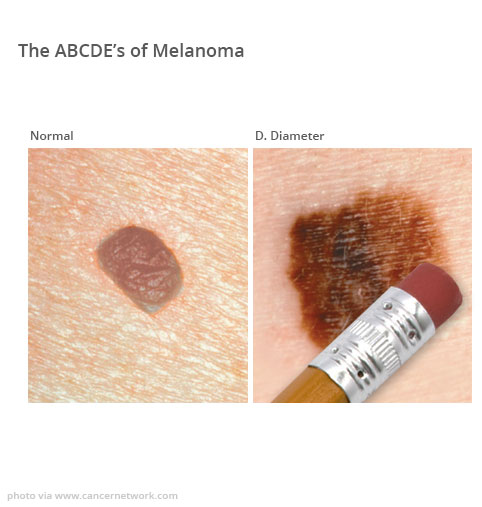
D. Diameter
Any mole that has a diameter larger than a pencil eraser is suspicious.
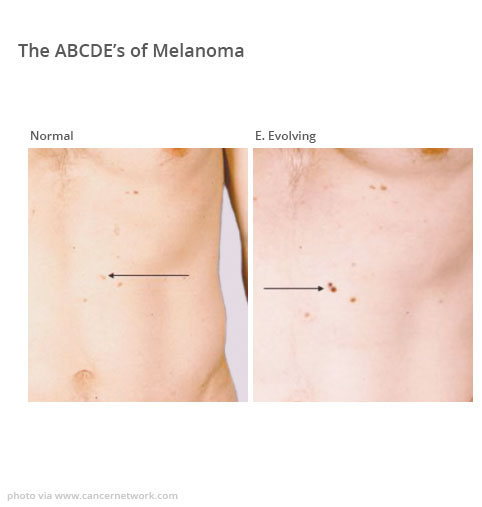
E. Evolving
Normal moles generally do not change appearance. Any mole that is growing larger, changing shape, or changing color is suspicious.

Professional Care
A mole that displays one or more of these characteristics should be evaluated by a dermatologist as soon as possible.
Skin cancer can be deadly, and postponing an evaluation can allow a cancerous mole to spread to nearby areas or to other parts of the body.

Overview
Warts are small, rough skin growths that typically occur on the hands and feet. They may occur singly or in multiples, and may spread to other parts of the body.
Warts are caused by the human papillomavirus (HPV) and are contagious.

Common Warts
Common warts typically occur on the hands, particularly on the knuckles and around the fingernails.
Common warts may bleed if picked, scraped, or cut, and usually contain small black dots, which are small, clotted blood vessels at the center of the wart.

Flat Warts
Flat warts are flat in shape, flesh-colored, and commonly occur in multiples. Flat warts typically appear on the face, neck, legs, and knees.

Plantar Warts
Plantar warts are hard, often painful lumps commonly found on the soles of the feet. They tend to be larger than common warts and are flesh-colored or brown with black specks.

Filiform Warts
Filiform warts are very small, thread-like warts typically found on the face, around the corners of lips and on the eyelids.

Genital Warts
Genital warts are caused by a type of sexually-transmitted HPV. These small warts can occur on the genitals, pubic area, and rectum, or inside the vagina in women.

Treatment
Many warts can be successfully treated with an over-the-counter salicylic acid solution. Other treatment options may include cryotherapy, blistering compounds, surgical excision, laser surgery, and immunotherapy.
Even with proper treatment, warts can be stubborn and may reoccur.