Surgical Dermatology
Nobody performs more surgical procedures on the skin than dermatologists. Nobody.
Board-certified dermatologists are highly trained skin surgeons performing thousands of procedures per year on nearly every body surface. From simple biopsies to complex surgical repairs, board-certified dermatologists have the experience and training to deliver optimal outcomes.
Regardless of whether you require removal of a benign growth or excision and repair of a large facial skin cancer, Clarus Dermatology should be your first stop. We will discuss medical and surgical options for treatment so you can select the one that best fits your care goals. Often, our physicians will perform the operation and reconstruction, but frequently we work with highly-vetted sub-specialists in otolaryngology, radiation oncology and plastic surgery to deliver the care that you need.
Common Skin Conditions Treated Surgically
While many skin conditions, such as acne, psoriasis, and rosacea, can be treated with our various medical services, some require surgical attention. At Clarus Dermatology, our experienced team routinely handles surgical procedures for common skin conditions, including:
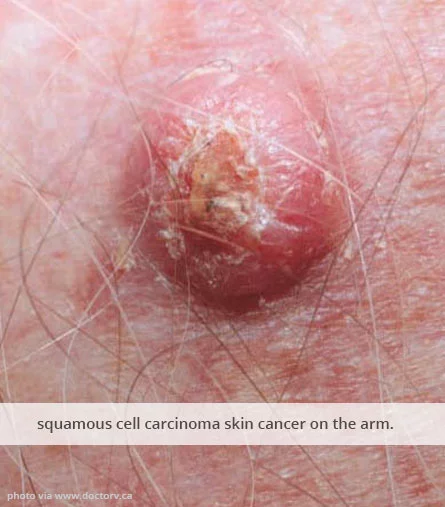
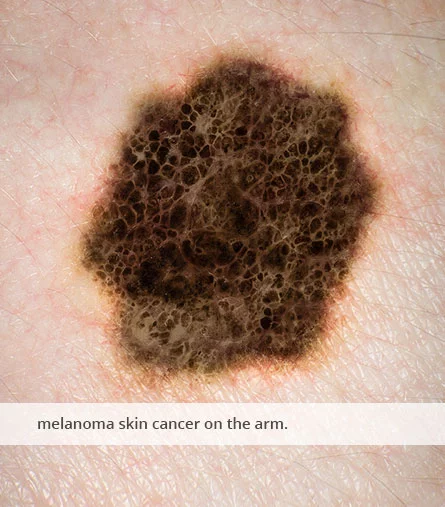
- Skin cancer, a disease involving the uncontrolled growth of abnormal cells in the outermost layer of the skin, called the epidermis
- Cysts, closed pockets of fluid that can vary in size and appear in various parts of the body
- Warts, small, benign (non-cancerous) skin growths caused by certain strains of the human papillomavirus (HPV)
- Moles, common skin growths that are usually harmless, but in some cases, can involve melanoma
- Keloids, thick, raised scars that can remain after the body heals from an injury
Benefits of Dermatologic Surgery
The benefits of dermatologic surgery vary based on the type of surgery you’re receiving. For example, suppose you’re having a cancerous patch of skin removed. In this case, the most notable benefit is the removal of the cancer, thus improving your overall health by minimizing the chances of it spreading.
Or, suppose you’re having keloids or noticeable warts removed. In this situation, the most noticeable benefit might be the cosmetic improvements. Once the area is removed, you can enjoy keloid- or wart-free skin.
Sometimes, the benefits might include minimized discomfort. For instance, suppose you have warts on your feet, causing pain when you walk. After removing them, you can enjoy walking without having the feeling of a painful pebble under your foot.
Dermatologists = Skin cancer experts
We are in the midst of an epidemic of skin cancer. If you or a loved one develops skin cancer of any type, we urge you to meet with our dermatologists. Our comprehensive approach involves three steps:
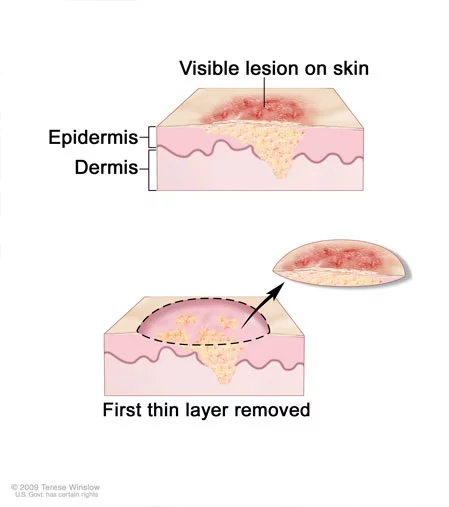
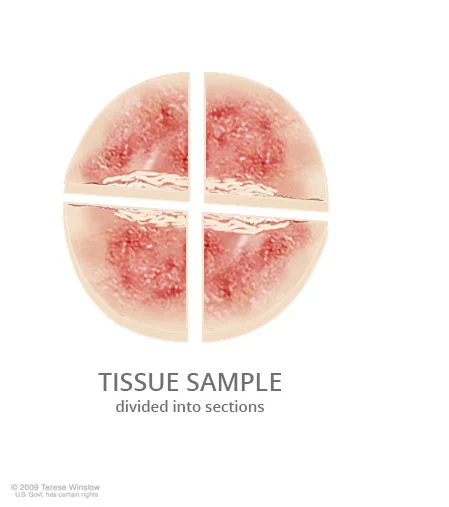
- Evaluation of the tumor.All dermatologists are trained as skin pathologists. As such, we are in a unique position to determine the best treatment options for you given the location, type, and subtype, of your tumor. We often review your pathology slides if we did not perform the diagnostic biopsy in-house.In contrast to many other practices, all Clarus dermatologists personally review each of their pathology specimens to ensure agreement with the outside pathologist’s assessment. This allows for superior “clinico-pathologic correlation” which leads to better outcomes for you. For example, often skin cancer can be treated by more conservative treatment strategies after review of the tumor itself.
- Evaluation of the patient. Before we choose the answers, we ask the questions. We put the particulars of your skin cancer into the context of your overall goals. How will your other medical conditions influence the healing process? Does your family history play a role? Are you healthy enough to undergo a major surgery with reconstruction? These are some of the questions that your dermatologist will consider when discussing treatment options with you.
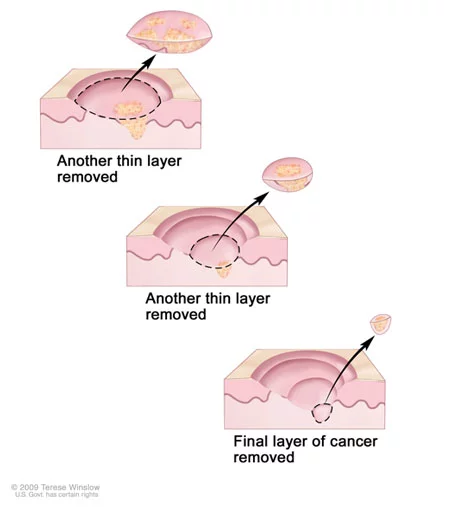
- Evaluation of your options. Although aggressive types of skin cancer surgery, like Mohs surgery, can be considered for many tumors, they often are not aligned with the patient’s care goals. We work with you to ensure that our recommendations respect your wishes.
- Completion of care. Once we have evaluated the tumor, the patient and his/her care goals we can proceed with treatment. Throughout this step you will be in the hands of an expertly trained, board-certified dermatologist and the entire Clarus care team.
Skin Surgery: What to Expect Before and After
The pre- and post-operative care involved with skin surgery can vary from one surgery to the next. For example, surgery to remove cancerous skin may require more prep and aftercare than a simple wart removal.
When you schedule a skin surgery with our team at Clarus Dermatology, we’ll always provide detailed instructions that give you a better idea of how to prepare and recover. If we need you to follow specific instructions before your surgery, we’ll provide them well before your scheduled surgery.
After your surgery, we’ll guide you through necessary post-operative care and offer more insights into what to expect from recovery. For simple surgeries, recovery periods may be short, if at all, but for more complex surgeries, it may take a bit longer to recover.
If you have any questions or concerns before, during, or after your surgery, don’t hesitate to ask—we’re here to help.
Pre-Operative Care for Skin Surgery
Generally, pre-operative care and preparation for skin surgery on your part is simple. We may provide a few straightforward instructions, such as avoiding shaving the surgical area and avoiding applying cosmetic products (makeup, lotions, or creams) to the area.
When you arrive for your surgery, we will prepare the surgical site, ensuring it is clean and ready for the procedure. If you have questions about what to expect from your particular procedure, feel free to ask.
Post-Operative Care and Recovery
After your surgery is complete, you may need to follow specific post-operative care instructions to ensure your surgical site heals smoothly. These instructions vary based on the surgery but might include things like keeping the wound and dressing dry for a set period or avoiding strenuous physical activity for a specific period.
Recovery times can vary, too. Some surgeries, such as a simple wart removal, might require little to no downtime. In contrast, other surgeries, such as skin cancer removal surgery, might require a few days to weeks of recovery and healing.
We will provide any specific instructions you’ll need to follow after surgery. If you have questions or concerns, don’t hesitate to contact our team. We’ll provide your surgeon’s number after the procedure, so if you have concerns, you can reach out to them, too.
About Skin Cancer
Frequently asked questions for surgical patients
What surgical services do you provide?
We provide a wide range of services including, but not limited to the following:
-Skin surgery on all body surfaces, including destruction of benign and malignant growths, excisional surgery, Mohs Micrographic Surgery, skin biopsy, scar revision including injection and resurfacing
Why can’t I schedule directly for surgery?
It is very important that we have adequate time to discuss the risks, benefits and alternatives of a given surgical approach with you before we schedule your procedure. Careful review of your existing pathology, medical history and care goals will determine the most appropriate treatment. Infrequently, additional biopsies must be performed prior to making a treatment recommendation.
Your pre-operative clinic visit ensures that our dermatologists have all of the information they need regarding your skin cancer, your medical history and your treatment goals to schedule the appropriate surgical procedure. It will also give you a chance to ask questions you might have about your condition and your treatment plan.
How should I prepare for my surgery?
While it’s not always easy to do when dealing with the time before a surgery, our best advice is simple: in a word: relax. In many cases, you will not need to make major changes during this time, but may have just a few simple instructions that you will need to follow in the hours just before your procedure.
Generally, most medications can be safely continued through your surgery, including blood thinners such as coumadin and aspirin. Refer to our detailed pre-operative instructions online for the procedure you’ll be having, or in the letter you received in the mail.
Who do I call if I have problems after my surgery?
Surgical complications do occur, but we are there for you 24/7. You will receive your surgeon’s cell-phone number at the time of surgery. We are there for you to ensure your post-operative course is as smooth as possible.