Eczema & Psoriasis Treatments
If you’re struggling with eczema or psoriasis, you’re not alone. Over 230 million people are navigating life with chronic, inflammatory skin conditions.
At Clarus, we help people understand the conditions they’re facing in-depth, from their underlying causes to treatment options. For the most personalized insights and tailored treatment, it’s worthwhile to schedule a consultation.
What is Eczema & Psoriasis?
Eczema and psoriasis are both inflammatory conditions that cause skin to itch and redden. Yet, their differences matter.
Eczema
The National Institute of Health (NIH) defines “eczema” as, “A group of conditions in which the skin becomes inflamed, forms blisters, and becomes crusty, thick, and scaly.” These visible symptoms are often accompanied by intense itchiness, or even burning.
Eczema has two underlying causes: an impairment of the skin’s epidermal barrier, and an overzealous immune system.
The impaired barrier can’t maintain moisture well, so skin dries and cracks. Irritants can then make their way past the skin’s outer layer to the dermis: the skin’s immune system layer. The immune cells in the dermis then overreact to the irritant, triggering an extreme inflammatory response.
Psoriasis
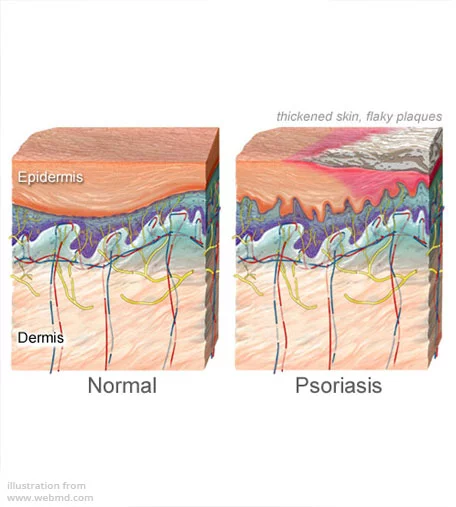
Psoriasis is an autoimmune condition: an inflammatory condition caused by the immune system attacking the skin. It’s “proliferative,” causing skin cells to grow and reproduce far more rapidly than they otherwise would.
This amplified growth outpaces the skin’s ability to shed dead cells. So, they accumulate, creating clumps of buildup called “plaques.”According to the NIH, the characteristic plaques of psoriasis are, “covered with silvery scales.”
Psoriasis also causes itching, burning sensations, soreness, cracks in skin that may bleed, and cyclic rashes.
First-Line Topical Therapies for Symptom Relief
Corticosteroids
Topical corticosteroids (TCs) suppress the immune system in a localized area. They vary by active ingredient, potency, viscosity, and application method. Ointments enable greater absorption than lotions.
The World Health Organization classifies TCs by strength, from Class I (most potent) to Class VII TC (least potent).
Only Class VII TCs, like 1% hydrocortisone, are available over the counter.
Eczema
TCs with Class VI – Class IV potency can effectively treat mild-to-moderate eczema symptoms on the face and thinner areas of skin.
Treating eczema on thicker skin, like the hands or soles of feet requires Class III ointments (or stronger).
Psoriasis
It is unusual to treat psoriasis with corticosteroids. Highly potent Class 1 TCs can effectively relieve psoriasis symptoms. But, they must be closely monitored, as they pose a high rise of side effects.
Calcineurin Inhibitors
Topical calcineurin inhibitors (TCIs) are creams and ointments that prevent the protein calcineurin from contributing to an eczema flare. They can be used on more delicate areas than corticosteroids (eyelids, neck), and some formulations can be used on infants.
TCIs can also be used to treat moderate-to-severe psoriasis on sensitive areas of skin. The highest potency TCIs are the most effective at alleviating psoriasis symptoms.
Vitamin D Analogs
Vitamin D compounds and analogs effectively regulate skin cells’ proliferation, differentiation, and cell death processes. The vitamin D pathways in the body also modulate inflammation. This can reduce or prevent the production of plaques.
As a result, vitamin D creams and ointments have become a first-line treatment for psoriasis.
Vitamin D ointments are not safe treatments for eczema.
 Moisturizers & Emollients
Moisturizers & Emollients
Moisturizers and emollients can keep skin hydrated, and some repair the skin barrier. Certain moisturizers and emollients include anti-inflammatory ingredients that can relieve itching and redness.
When choosing ointments, look for products with the National Eczema Association’s (NEA) Seal of Acceptance™, or The National Psoriasis Foundation’s Seal of Recognition.
Customized skincare options
While there is a wide range of skincare treatment options available, the best treatment varies from person to person. That’s why it’s important to work with a dermatologist to develop a skincare routine customized to your skin’s needs.
 Advanced Light Therapy for Eczema & Psoriasis
Advanced Light Therapy for Eczema & Psoriasis
Narrowband UVB phototherapy is an effective treatment for psoriasis, including severe psoriasis. It’s safe enough to be used by children, women who are pregnant, and people who are immunocompromised.
Because ultraviolet light therapy can stimulate vitamin D production, it has had mixed results as an eczema treatment. Some people find it has no effect, or even worsens the condition.
 Advanced Systemic & Biologic Medications
Advanced Systemic & Biologic Medications
Systemic and biologic medications are oral or injectable antirheumatic treatments.
Immunosuppressants
Immunosuppressants prevent the immune system from attacking the skin (psoriasis) or overreacting to stimuli (eczema flare). Most immunosuppressants are Disease-Modifying Antirheumatic Drugs (DMADs) and calcineurin inhibitors.
Biologics (Inflammatory Cytokine Inhibitors)
Biologics are a relatively newer class of drugs. They’re called “biologics” because they’re derived from living organisms.
Most biologics are targeted monoclonal antibodies. They bind to specific cytokines in the immune system to modify the system’s response.
Dermatologists will typically use a cytokine panel before prescribing a biologic. It identifies which type of cytokine is malfunctioning in a patient’s body with greater precision, and ensures the prescribed biologic targets it.
Even with a cytokine panel, a biologic may not be the right treatment for every person. Personalized treatment is key.
Daily Skincare & Lifestyle Tips
Daily skincare routines, diet, and exercise, are as important as prescription medications to treating psoriasis and eczema effectively. But, not all changes lead to positive results.
Skincare Tips
Reduce the frequency and severity of your symptoms with these tips.
- Use gentle, fragrance-free cleansers when cleaning your skin and your clothes.
- Bathe or shower in lukewarm water, not hot water.
- After a bath, pat your skin dry and apply a moisturizer immediately.
- Choose products highly rated by skin condition advocacy organizations
- National Eczema Association (NEA) Seal of Acceptance™
- National Psoriasis Foundation (NPF) Seal of Recognition™
Diet & Hydration
Anti-inflammatory diets can reduce the frequency and severity of symptoms of inflammatory conditions. The National Eczema Association has published a free resource on the optimal diet for eczema symptom relief. Likewise, the National Psoriasis Foundation offers a similar, psoriasis-oriented guide online.
Dehydration worsens both psoriasis and eczema, so it’s wise to drink enough water, proactively, throughout the day. Hydrate, but avoid overhydration; it throws off your body’s electrolyte balance.
 Stress Management
Stress Management
Stress can trigger and worsen inflammation. To better manage stress, make sure to get 7+ hours of sleep nightly, exercise daily, connect with loved ones, and engage in mentally-healthy habits (i.e. meditation, journaling).
Expert Care with Proven Results
The best psoriasis and eczema care is provided by specialists. At Clarus, our team is composed of board-certified specialist dermatologists and clinically-trained Masters of Dermatology Physician Assistantship.
All of our practitioners have access to innovative therapeutic technology—like our state-of-the-art Daavlin, narrow-band UVB phototherapy cabinet.
To learn more about our team and the treatment options we offer, book a consultation online. Or, give our office a call during regular business hours: (612) 213-2370.
Frequently Asked Questions
Eczema is a condition caused by an overzealous immune system, similar to asthma or allergies. It’s noncontagious, and it’s characterized by redness of the skin, severe itching, oozing, and/or scaly rashes. To learn more about it, we invite you to read our guide, “How Do You Get Eczema?”
In contrast, psoriasis is an autoimmune condition. The immune system gets confused and attacks the skin instead of pathogens or other external threats.
While psoriasis skin reddening, inflammation, and itchiness, it is mainly characterized by the rapid buildup of skin cells (“skin plaques”). It requires different treatments than eczema does.
To learn more, check out our guide, “Psoriasis Management: Effective Strategies For Clearer Skin.”
Not exactly. Unfortunately, there is currently no permanent “cure” for either psoriasis or eczema. Fortunately, effective treatments can significantly reduce symptoms.
Biologic treatments target specific immune system cells called “cytokines,” suppressing or disrupting their functions. This can reduce the severity and frequency of the immune system’s symptom-causing responses.
Yes. However, it’s important to work with a specialist dermatologist who can determine the appropriate type of light therapy for your condition.
Several factors affect how soon a psoriasis or eczema treatment achieves results, including:
- The condition’s severity
- The condition’s precise underlying cause in a given patient
- The type of treatment
Results vary based on the severity of the condition and the treatment used.
Yes. For lifestyle strategies, read our expert guides, “The Role of Diet In Maintaining Healthy Skin,” “Why Your Skincare Routine Isn’t Working” and, “How To Treat Psoriasis and Eczema In Cold Weather? 6 Tips From A Dermatologist.”
Of course, no two people have identical needs when it comes to clinical skin care. That’s why it’s so important to work with a dermatologist directly: it’s the best way to find an effective treatment tailored to your needs.