Medical Dermatology
Expert, personalized skin condition treatment & care
What Is Medical Dermatology?
Medical dermatology is a sub-specialization of dermatology focused on diagnosing and treating health conditions that affect (or originate in) the skin.
Dermatology is a field of medicine specializing in skin, scalp, hair, and nails. Focused clinical dermatology research deepens our understanding of these aspects of the body: their underlying structures, their functions, and the nature of conditions and disorders that affect them.
With those insights, a dermatologist can specialize in medical care or cosmetic intervention.
Cosmetic Dermatology Vs. Medical Dermatology
Both cosmetic dermatologists and medical dermatologists are board-certified physicians. All dermatologists can prescribe pharmaceutical medications, advanced therapies, and even surgical intervention when it’s the best treatment option.
Yet, cosmetic and medical dermatologists differ.
Cosmetic dermatologists focus on beauty. They’re clinically trained experts in the art of aesthetics. For any threat to diminish the beauty of a person’s skin—be it discoloration, dandruff, or wrinkles—cosmetic dermatologists offer effective, therapeutic interventions.
In contrast, medical dermatologists focus on health. We, too, are clinically trained experts in an art: the art of diagnosing and treating medical conditions affecting the skin.
Medical Dermatologists’ Expertise
Medical dermatologists treat acute and chronic skin conditions alike. That includes skin cancers. With cutting-edge technology, we can even diagnose precancerous skin lesions—often early enough to fix them before a single symptom is felt.
If you’re dealing with new, acute skin or scalp symptoms—whether it’s boils, blisters, folliculitis, or lesions—we’re the right professionals to see. Medical dermatologists can diagnose an acute allergy, skin infection, or something more serious; then, we get our patients exactly what they need to knock the problem-causers out.
We’re also uniquely equipped to diagnose and treat chronic conditions. Recurring issues like acne, warts, or hives are deceptively simple; yet, their treatment must be precise to be effective. Immune-centric skin disorders, psoriasis, and eczema, are even more complex.
Fortunately, as medical dermatologists, we have the power to offer real relief and healing from conditions across that severity spectrum.
Medical Dermatologists Can Help You Today
Whether you’re concerned about chronically painful or itchy skin, pitted and brittle nails, or even melanoma, our medical dermatologists are here to help.
We can get your skin healing and your health feeling good. We also offer regular skin wellness checks and preventative screenings. No matter your skin’s condition, connect with us today.
Acne Treatment
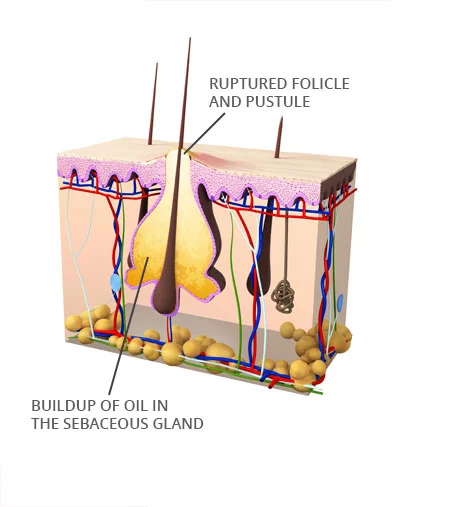
When one of the skin’s pores becomes clogged, it can swell into a bump called a comedo or pimple. Typically, it’s clogged by dead skin cells or excess sebum—an oil the skin produces as a protective, moisture-retaining barrier. It can also be clogged by keratin, a protein the body uses to make hair, nails, and the skin’s epidermis, or by microbes on the skin’s surface.
When a person has more than a few pimples on their skin or scalp, they have acne.
Types of Acne
Acne is fairly common. A case of acne is often composed of different types of comedones.
Common Acne (Acne Vulgaris)
If clogged pores aren’t inflamed, they’re typically blackheads (clogged pores with dark, oxidized melanin cells) or whiteheads (covered clogged pores). Mild inflammation causes papules (tender, raised bumps).
 Pustular Acne & Cystic Acne
Pustular Acne & Cystic Acne
If the clog contains an irritant or pathogen (bacteria or fungus), the pore typically becomes more intensely inflamed. The body’s immune system sends white blood cells to the site, which can fill the pore with pus, creating pustules or cysts.
Nodular Acne
Certain conditions can cause the immune system’s and sebaceous glands’ response to inadvertently create nodules. The influx of immune cells and thick sebum worsen the pimple until it ruptures the pore, spreading the bacteria and embedding the clog deeper in the skin.
Nodular acne is often the most challenging to treat.
How Dermatologists Treat Acne
Our dermatologists first determine the precise nature and cause of a person’s acne.
We ask questions and take detailed notes to learn about a patient’s medical history, conduct a visual physical exam, and we may perform a swab analysis or blood panel to better understand pathogenic or hormonal factors.
Once we have the information we need, treatment can begin. No two cases of acne need identical treatment. Instead, treatment should be tailored precisely to target the core problem, personalized to best alleviate symptoms, and built to minimize side effects.
The most common treatments target bacteria and inflammation with:
- Antibiotics
- Topical erythromycin or clindamycin
- Oral tetracyclines or sulfamethoxazole
- Antiseptics
- Topical benzoyl peroxide, salicylic acid, or azelaic acid
- Retinoids (Vitamin A Compounds)
- Topical Tazarotene, tretinoin, or adapalene
- Oral isotretinoin
- Hormone Modulators & HRT
- Topical androgen inhibitors i.e. clasccoterone or spironolactone
- Oral spironolactone
- Oral synthetic progestin + estradiol (drospirenone, norgestimate, or norethindrone w/ ethyl estradiol)
- Medical Extraction
- Chemical Peels
- Light Therapy
- Photodynamic therapy (PDT)
- LED light therapy
- Laser light therapy
- Fractional CO2 laser
- Diode laser
Tips To Manage Acne and Prevent Scarring
To manage acne and prevent scarring, maintain a gentle skincare routine. Keep your skin moisturized and free from irritants or bacteria. Use plenty of sunscreen.
When you have a pimple, treat it gently with topical cleansers, or with any medications your dermatologist has prescribed. To remove it, use a skin-safe method like a pimple patch to prevent scarring or the spread of bacteria. The compress method can also drain a pimple safely, but you must use sterile water and cloth.
If you need to remove a pimple quickly, seek a dermatology professional who can drain and extract it using sterile tools and minimal incision.
By far the best way to manage your acne effectively is to consult a dermatologist. Early intervention, targeting the specific type of acne affecting you, is key to long-term skin health.
Eczema & Dermatitis Treatments
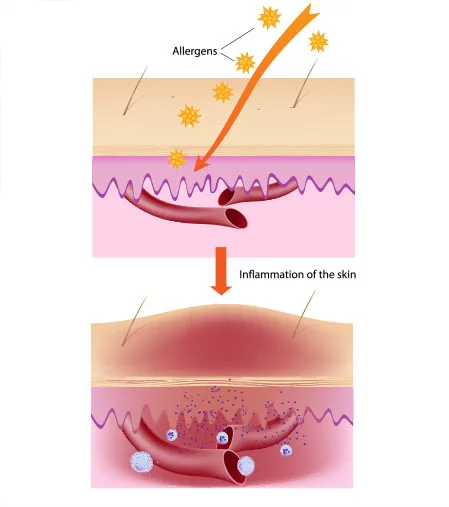
Eczema and dermatitis are conditions caused by an overzealous immune system.
The immune system overreacts to irritants or potential threats on the skin, causing inflammation, redness, intense itching, burning, and blisters. Dermatitis is a term for the inflammation and sores on the skin associated with eczema.
Most types of eczema have two underlying causes: an impairment of the skin’s epidermal barrier, and an overzealous immune system.
When the epidermal barrier isn’t functioning well, it can’t effectively maintain moisture and protect the skin from irritants. This leads to dryness and cracking, letting irritants make their way past the skin’s outer layer to the dermis: the skin’s immune system layer.
The immune cells in the dermis then overreact to the irritant by triggering an inflammatory response: an eczema flare-up.
Types of Eczema
There are several types of eczema. The most common is “atopic dermatitis,” wherein the eczema response manifests as an itchy rash and dry, scaly patches. The patches can thicken and harden over time.
Other forms of eczema cause different inflammatory responses. For example:
- Nummular eczema. It causes circular, itchy patches, which may ooze.
- Dyshidrotic eczema. This causes itchy blisters, typically on the hands and feet.
- Seborrheic dermatitis. It causes raised bumps, rashes, and itchy skin flakes on parts of the body with sebaceous glands (like the scalp).
- This causes the glands to overproduce oil, creating greasy patches and dandruff.
Different types of eczema require different approaches to treatment. As a result, it’s important to get an accurate, specific diagnosis and personalized treatment.
Diagnosing Eczema
To diagnose eczema, a dermatologist begins by asking questions about your medical history, any history of eczema or asthma in your family, and environmental factors that might be contributing to your symptoms.
Then, the dermatologist will visually inspect the affected skin. They may perform a patch to pinpoint contact triggers and rule out allergies. An IgE blood panel might also be recommended, to gain precise information about the body’s immune response.
These tests are the gold standard for eczema diagnosis; further tests, like biopsies, are rarely helpful or necessary.
Treating Eczema
Eczema is best treated with steroids, calcineurin inhibitors, or biologics.
 Corticosteroids
Corticosteroids
Topical corticosteroids of low-to-moderate potency (methylprednisolone, hydrocortisone, etc.) can effectively treat mild-to-moderate eczema symptoms on the face and thinner areas of the skin.
To treat eczema on thicker skin, dermatologists often prescribe stronger steroid ointments, like betamethasone. Oral steroids may be prescribed to treat acute, severe symptoms.
Calcineurin Inhibitors
Topical calcineurin inhibitors (TCIs) prevent the protein calcineurin from contributing to an eczema flare. They can be used on more delicate areas than corticosteroids (eyelids, neck).
Biologic Monoclonal Antibodies
The biologic drug Dupixent® (dupilumab) is FDA-approved to treat moderate-to-severe eczema in adults and children over age 6. It targets cytokines, the immune system’s messenger cells.
Dupilumab intercepts the “message” these cells send to the rest of the immune system, interrupting and preventing the system’s overactive, inflammatory response to irritation. This reduces the severity of eczema flares, and it can prevent them altogether—without suppressing any of the other functions of the immune system.
Eczema Management & Prevention
To reduce the frequency and severity of eczema flares, cultivate a gentle skincare routine. Use daily moisturizers and emollients that include anti-inflammatory ingredients, which relieve itching and redness.
When choosing skincare products, look for lotions and moisturizers with the National Eczema Association (NEA) Seal of Acceptance™.
Other eczema management strategies include drinking enough water, sticking to an anti-inflammatory diet, getting 7-9 hours of sleep each night, and taking up stress reduction practices.
To learn more about our approach to eczema treatment, please see our Psoriasis & Eczema Treatment Services page.
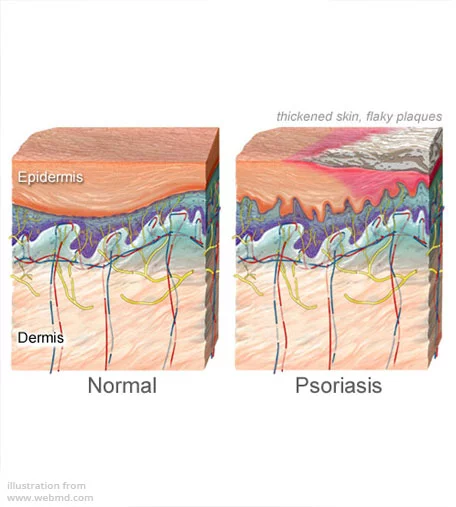
Psoriasis Management
Psoriasis is an autoimmune condition where the immune system attacks the skin. It’s characterized by inflammation, redness, and the buildup of scaly skin cells called plaques.
To learn more about what causes psoriasis, and our approach to psoriasis diagnosis and treatment, please see our Psoriasis & Eczema Treatment Services page.
In addition to medical treatment, people with psoriasis can improve their condition by adopting a psoriasis-friendly skincare routine, staying hydrated, sticking to an anti-inflammatory diet, and practicing stress management.
Rosacea Treatments
Rosacea is a chronic, inflammatory, skin-reddening condition with multiple underlying causes. It cannot be cured. However, 70% – 90% of people with rosacea find symptom relief and report effective rosacea management with the right treatment.
The most characteristic symptoms of rosacea are persistent facial redness, chronic facial “flush” that can feel hot or painful, small red bumps on the affected skin, and visible red blood vessels.
Rosacea inflammation can also affect the eyes. This effect, called ocular rosacea, can make eyes feel itchy, burning, or gritty, often causing them to water. Many people dealing with ocular rosacea experience blurry vision and blepharitis—inflamed eyelids that develop crusts at the base of the eyelashes.
The most severe rosacea cases can cause hyper-reactive dilation of blood vessels, skin overgrowth (called “rhinophyma” on the nose), and the overgeneration or enlargement of sebaceous glands—glands that produce a protective oil that, in moderation, keeps the skin moisturized and elastic.
Causes Of Rosacea
While rosacea has been extensively studied, we still haven’t determined the exact underlying causes of the condition. Nevertheless, we’ve discovered specific exacerbating factors (and potential causes).
Microbiome Factors
- An overabundance of pathogenic bacteria, including Staphylococcus epidermis, Bacillus oleronius, and Cutibacterium acnes
- An abnormal response to bacteria by the skin’s immune receptors
- Higher-than-typical concentrations of Demodex mites hosted in the Sebaceous
Vasculature Factors
- Heightened blood vessel fragility
- Over-dilated or enlarged blood vessels
- Increased blood flow
- Hyperactive neurovascular system
Immune System Factors
- Unusual or over-active T-cell mediated response
- Interactions between adenosine triphosphate (ATP) and inflammatory pathways are atypical
- Overproduction of defense peptides and inflammatory cells
Current research hasn’t definitively shown any of these factors to be the cause of rosacea. Still, effective treatments address these factors.
Diagnosing Rosacea
Medical dermatologists diagnose rosacea by observing the individual’s condition during an exam, and by ruling out conditions with similar symptoms. For example, lupus can present similarly to rosacea, so a physician might take a blood test to rule it out.
If you come to a dermatologist with rosacea symptoms, we will ask you about your medical history.
Then, we’ll use a dermatoscope to examine the affected skin, using its magnifying lens and polarized light to get a clear image of its pattern and structure. The scope makes it easier to recognize telltale signs of rosacea, like blood vessels arranged in repeating polygon shapes.
During the exam, a dermatologist might use a type of biomicroscope called a “slit lamp” to inspect your eyes. This is one of the safest, non-invasive ways to discern evidence of ocular rosacea.
We might also perform optical coherence tomography or reflectance confocal microscopy scans, particularly if we suspect Demodex mites are an exacerbating factor.
A skin biopsy is another diagnostic option. While more invasive, it can also offer insights into the condition’s specific effects on the skin. Ultimately, though, dermatologists want to get the information necessary to understand your skin, without irritating it.
Rosacea Treatments
There’s no cure for rosacea. But, there are several treatment options that effectively reduce the severity and impact of symptoms.
Treatments address the known factors in rosacea severity. These include:
- Anti-Parasitic Medications (Anthelmintics)
-
- These medications target Demodex mites in the skin’s microbiome.
- Ivermectin 1% cream
- Permethrin cream 5%
- Praziquantel
- Topical benzyl benzoate (BB) and crotamiton
- These medications target Demodex mites in the skin’s microbiome.
- Monocarboxylic & Dicarboxylic Acids
- Topical acids simultaneously stimulate mitochondria and modulate the skin’s receptors, pathways, and inflammatory cell production, normalizing the skin’s immune response.
- Azelaic acid
- Tranexamic acid
- Linoleic acid
- Topical acids simultaneously stimulate mitochondria and modulate the skin’s receptors, pathways, and inflammatory cell production, normalizing the skin’s immune response.
- Antibiotics
- These medications reduce or eliminate bacteria on the skin.
- Oral doxycycline
- Oral minocycline
- Topical metronidazole
- Azithromycin eye drops (for oracular rosacea)
- Erythromycin eye drops (for oracular rosacea)
- These medications reduce or eliminate bacteria on the skin.
- Topical Vasoconstrictors
- These creams and gels target blood vessels to reduce redness and flushing.
- Brimonidine
- Oxymetazoline
- These creams and gels target blood vessels to reduce redness and flushing.
 Oral Beta Blockers
Oral Beta Blockers
- These medications lower blood pressure to indirectly reduce redness, flushing, and stress on fragile capillaries.
- Carvedilol
- Propranolol (used in combination with doxycycline)
- These medications lower blood pressure to indirectly reduce redness, flushing, and stress on fragile capillaries.
- Retinoids
- These vitamin A derivatives modulate the immune system and inhibit cell overgrowth to prevent inflammation and rhinophyma.
- Isotretinoin (low dose)
- These vitamin A derivatives modulate the immune system and inhibit cell overgrowth to prevent inflammation and rhinophyma.
- Red Light Therapy
- This therapy stimulates mitochondria in cells to improve blood flow, reduce oxidative stress, and increase production of collagen and anti-inflammatory mediators.
- Photodynamic & Laser Therapies
- These therapies destroy targeted tissue, cells and blood vessels to reduce skin redness, inflammation, hyperactive blood vessel dilation, and rhinophyma.
- Pulsed dye lasers (PDL)
- CO2 lasers
- Erbium YAG lasers
- Intense pulsed light (IPL)
- Photodynamic therapy (PDT)
- These therapies destroy targeted tissue, cells and blood vessels to reduce skin redness, inflammation, hyperactive blood vessel dilation, and rhinophyma.
- Meibomian Gland Probing (MGP)
- This intervention treats ocular rosacea.
- Electrosurgery
- Electrosurgeries remove blood vessels and resurface skin to alleviate rosacea symptoms.
- Electrocoagulation
- Electrosection
- Dermabrasion (for rhinophyma)
- Electrocautery (for rhinophyma)
- Electrosurgeries remove blood vessels and resurface skin to alleviate rosacea symptoms.
Managing Rosacea
To manage rosacea symptoms, take proactive action to prevent flare-ups and exacerbations. Use sun protection (SPF 30 or higher), avoid overheating, and engage in stress-reducing practices.
Wart Removal
“Warts are prevalent benign lesions caused by the human papillomavirus (HPV) that occur in the mucosa and skin.”
—NIH Medical Encyclopedia
Warts are non-cancerous growths on skin. When the HPV virus infects the outer layer of skin, it causes excess growth of keratinocytes, a type of skin cell, and an overproduction of the keratin protein. Keratin builds up around the HPV’s point of infection, creating the wart.
While they’re not lethal, the worst warts can lead to secondary infections. These warts break the skin barrier, opening the door to bacteria like A streptococcus and MRSA. HPV warts can also impair or deplete Langerhans cells (LCs), which typically alert the immune system to pathogens attacking the skin. By damaging and diminishing LCs, the virus protects itself—making it challenging to kill.
The most characteristic symptom of warts is the keratin growth. Other symptoms tend to be type-specific, largely associated with warts in a particular location or with a distinct composition. The most common wart types are:
 Common Warts
Common Warts
- Raised bumps
- Grainy or “cauliflower-like” texture
- Usually found on the face, arms, hands, legs, or feet
- Typically caused by HPV types 2 or 4
- More rarely caused by types 1, 3, 27, 29, or 57
- Painful when subject to friction
- Often dotted with clotted blood vessels
- Raised bumps
- Flat Warts
- Raised, non-painful bumps
- Smooth texture
- Usually found on the face, arms, hands, legs, or feet
- Typical caused by HPV types 3, 10, 28, and 49
- Often pink or matching the skin’s color
- Raised, non-painful bumps
 Plantar Warts
Plantar Warts
- Hard, painful or tender growths
- Grainy or callus-like texture
- Only found on the soles of feet
- Typically caused by HPV types 1, 2, 4, 27, and 57
- Often skin-colored, dull gray/brown, or dark purple, dotted with clotted blood vessels
- “Mosaic warts” are tight clusters of plantar warts on the ball or heel of the foot.
- Hard, painful or tender growths
- Genital Warts
- Raised bumps
- Rough or “cauliflower-like” texture
- Found on skin and mucous membranes of the genitals, rectum, or mouth / throat
- Typically caused by HPV types 6 and 11
- More rarely caused by types 16, 18, or 52
- Rarely painful or itchy
- Often skin-colored or white, dotted with clotted blood vessels
- Raised bumps
 Filiform Warts
Filiform Warts
- Softer, flexible thread-like strands projecting from skin
- Spiky or “brush-like” texture
- Usually found on the neck or face, often around the eyes, nose, or lips
- More rarely found on arms, hands, or legs
- Typically caused by HPV types 1, 2, 4, 27, and 29
- Not painful
- Often skin-colored, pink, or yellow
- Softer, flexible thread-like strands projecting from skin
- Periungual Warts
- Hard bumps
- Rough or “cauliflower-like” texture
- Only found near or under fingernails and toenails
- Frequently painful and can bleed easily
- Typically caused by HPV types 1, 2, 4, 5, 7, 27, and 57
- Often start out translucent or skin-colored
- Can turn yellow or gray over time
- Hard bumps
Diagnosing Warts
In the vast majority of cases, a dermatologist can diagnose a wart simply by looking at it closely. On rare occasions, they might perform a shave biopsy to rule out a more dangerous condition (like skin cancer).
If the wart is in the rectum or cervix, it should be treated by a proctologist or gynecologist (respectively), rather than a dermatologist.
Very rarely, the dermatologist may refer you for an HPV genotyping test, if there are signs it’s a high-risk strain. The wide majority of HPV types are low-risk.
Wart Treatment Options
While some warts heal on their own without intervention, this can take over a year. Dermatologists usually aim to treat warts and the underlying infection at once.
Most wart treatments involve physically removing the entire growth, either by chemically breaking down the keratin composing the wart, or by targeting and destroying the wart’s HPV.
Physical Wart Removal
To physically remove a wart, physicians usually freeze it with liquid nitrogen (cryotherapy), burn it with an electrical current (electrosurgery) or concentrated light radiation (laser ablation), or scoop it out with a curette (surgical excision). These methods penetrate down to the warts’ bottom-most layer, destroying it entirely to reduce the risk of recurrence.
Physical wart removal interventions are outpatient, and most are performed in the dermatologist’s office using local anesthetic.
Laser ablation electrosurgery, and surgical excision often completely remove the wart(s) in a single session, while cryotherapy wart removal takes 2-6 sessions, on average. People typically wait 1-3 weeks between each cryotherapy session for the nitrogen to take full effect.
Chemical Wart Treatment
“Chemical wart treatment” is an umbrella term for all medical, chemical compounds used to destroy warts. Treatments may apply chemical compounds to wart surfaces, inject those compounds, or utilize those chemicals for a therapeutic “peel.”
There are six categories of chemical compounds used to treat warts.
- Keratolytic agents soften or dissolve the wart’s structural keratin.
- Vesicants (blistering compounds) kill wart cells, then push the remaining wart out of the skin.
- Retinoids (vitamin A derivatives) disrupt the growth of wart cells and promote exfoliation.
- Immunomodulators (immune response activators) stimulate the body’s immune response, helping it target and destroy the wart-causing HPV.
- Cytotoxic glycopeptide antibiotics destroy wart tissue by disrupting the structure and function of the wart’s cells.
- Antivirals interfere with HPV’s replication (reproduction) and strengthen the immune system’s response against it.
Chemical | Type | Application Options | Typical Use Cases | Notes |
Salicylic acid | Keratolytic agent | OTC topical gel Chemical peel | Common warts Plantar warts Filiform warts Periungual warts | Most common chemical wart treatment |
Podophyllotoxin (or, podophyllum resin) | Keratolytic agent | Prescription topical gel | Genital warts Plantar warts (podophyllum resin only) | Gel is applied 2x daily for 3 days, then skipped for 4 days. Repeat for 2-4 weeks. |
Trichloroacetic acid (TCA) | Keratolytic agent | Prescription topical gel Chemical peel | Genital warts Common warts Periungual warts Plantar warts | Applied once per week for 4-6 weeks |
Glycolic acid | Keratolytic agent | OTC topical gel (combined with salicylic acid) Prescription topical gel Chemical peel | Plantar warts Filiform warts Flat warts Common warts | Second most-common chemical wart treatment |
Sulfur | Keratolytic agent | OTC topical ointment | Flat warts | Only effective in mild cases |
Cantharidin | Vesicant | Prescription topical gel Chemical peel | Common warts, Plantar warts, Periungual wart | Blister forms in 24-48 hours, and heals in 4-7 days. Use with caution (blisters can spread HPV). |
Tretinoin | Immunomodulator & Immune Response Activator | Prescription topical cream Chemical peel (“immunopeel” or “face peel”) | Genital warts Plantar warts Filiform warts Common warts on face | Effective treatment of recalcitrant warts affecting immuno- compromised and immuno- suppressed people |
Cimetidine | Immunomodulator & Immune Response Activator | Prescription oral tablet Prescription topical gel | Common warts Plantar warts Periungual warts Flat warts Filiform warts | Used to treat recalcitrant warts in pediatric patients |
Cidofovir | Antiviral | Intralesional injection Prescription topical cream | Common warts Plantar warts Periungual warts Flat warts Filiform warts | Used to treat recalcitrant warts in children and immuno- compromised people |
Acyclovir | Antiviral | Intralesional injection Prescription topical ointment | Periungual warts Plantar warts | Apply ointment 5-6x daily for 7 days. |
Managing & Preventing Warts
Many HPV strains are highly contagious.
While genital warts are only passed on sexually, common warts are caused by more communicable papillomaviruses. Wart-causing HPVs can be transmitted skin-to-skin and via droplets, letting them spread quickly by handshakes, wet bath mats, or simply accidentally touching an infected area.
Fortunately, studies suggest only 40-44% of people who contract HPV end up developing warts. Often, the immune system can kill or contain HPV before you experience any symptoms.
Stop The Spread With Hygiene & Disinfection
When you’re dealing with a wart, limit your risk of reinfection and prevent its spread to others. Don’t scratch or pick at it. Instead, put a bandage over the wart while treating it.
Limit your risk of catching HPV from someone else by periodically washing your hands with soap and running water. Note that alcohol-based sanitizers don’t kill HPV.
Slow or prevent the spread of HPV in common areas with effective sanitization. Use bleach or hydrogen peroxide to disinfect communal showers, locker rooms, and other damp areas particularly conducive to the spread of plantar warts.
Help Your Immune System Fight HPV
Immunocompromised people are more likely to have chronic or recalcitrant warts than others.
One of the best preventative strategies is to give your immune system a boost. Eat nutrient-rich foods, take antioxidant supplements, get 7-9 hours of sleep per night, and engage in stress-reducing practices.
It’s also smart to get the 9vHPV vaccine (also called Gardasil). It helps your immune system protect you from nine HPV variants, including strains known to cause genital warts and cervical cancer.
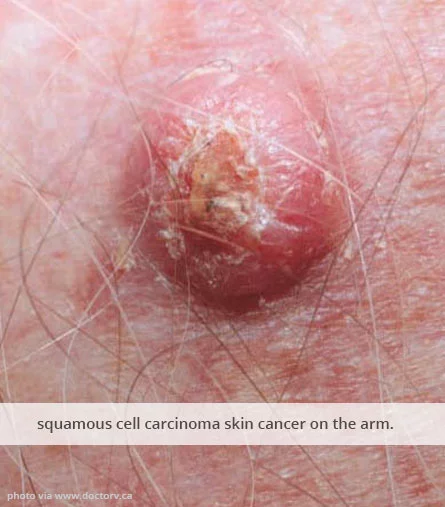
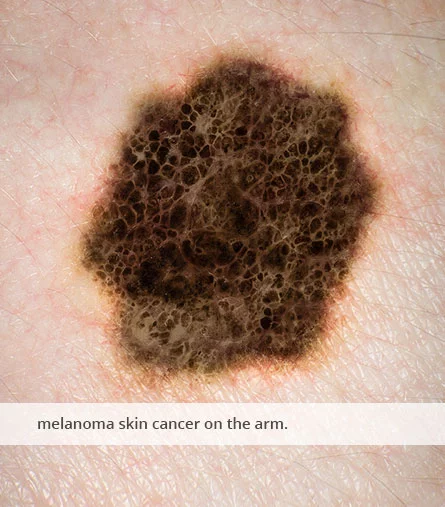
Skin Cancer Screenings & Treatment
Skin cancer treatment is one of the most urgent types of medical dermatology care.
We strongly recommend all adults get a full-body skin cancer screening by a board-certified dermatologist annually. Those who face a higher risk of skin cancer (due to other medical conditions or their family histories) should attend screenings 2-4 times per year.
To learn more about our approach to skin cancer screenings, diagnosis, and treatment, please see our Skin Cancer Services page.
In addition to professional dermatology services, you can make choices that reduce your risk of skin cancer. Wear protective clothing and sunscreen when you’re outside, skip tanning in favor of UV-free alternatives, and perform a skin cancer self-check once per month.
Skin Infection Treatment
“[A rash is] an area of the skin that has changes in texture or color and may look inflamed or irritated. The skin may be red, warm, scaly, bumpy, dry, itchy, swollen, or painful. It may also crack or blister.”
—NIH Dictionary
Rashes may be caused by skin autoimmune conditions, allergic reactions, heat, or skin infections.
Types of Rashes
Autoimmune Rashes
Autoimmune conditions can cause rashes when the immune system malfunctions and attacks the skin. Of these conditions, the most likely to result in rashes are:
- Lupus
- Psoriasis
- Dermatitis herpetiformis
- Dermatomyositis
- Sjögren’s syndrome
- Pemphigoid
- Scleroderma
A dermatologist may be able to diagnose an autoimmune condition by examining your skin. But, many autoimmune conditions affect multiple systems of the body. An autoimmune specialist like a rheumatologist will be better able to offer insights and effective treatment.
 Allergy-Induced Rashes
Allergy-Induced Rashes
When a rash happens after contact with an allergen, it’s an allergic reaction.
Some substances, like the urushiol oil on poison ivy leaves, or bioactive proteins in a mosquito’s saliva, are near-universal allergens. In contrast, only 1 out of 3 adults’ immune systems react to pollen as an allergen, and 1-2% are allergic to peanuts.
The most common allergy-induced rashes are:
- Hives (raised itchy welts, usually skin-colored or pink)
- Bug bites (raised, itchy, red, inflamed bumps at the site of the bite)
- Contact dermatitis (itchy, peeling, inflamed, blistering skin, sometimes generating sores or skin ulcers)
When a person experiences dermatitis without a contact trigger, it’s usually atopic dermatitis.
Most types of dermatitis are categorized as eczema, a condition similar to asthma or allergies. Eczema is the result of an overzealous immune system, though the immune system doesn’t attack the skin. [To learn more about diagnosing and treating it, explore our eczema services page.]
Heat Rashes
“Heat rash,” is the common term for miliaria, the inappropriate backflow of sweat into the skin, causing sweat-filled blisters to form in the epidermis (or, more rarely, the dermis).
Miliaria happens when sweat glands and ducts are blocked, typically by sweat that’s already been secreted but has nowhere to go. Clothing traps pooling sweat against the skin, ultimately causing the sweat blisters, redness, and inflammation.
More rarely, the glands and ducts are blocked by a biofilm created by bacteria, inflamed or scaly skin buildup due to psoriasis, medications, or strong antiperspirants.
Heat Rashes vary in severity, but most can be treated by simply cooling down.
Skin Infections
A skin infection is an inflammatory process affecting the skin, involving the microbial invasion of the layers of the skin and underlying soft tissues. Skin infections vary in presentation and severity.
Most skin infections are caused by bacteria, viruses, parasites, or fungi.
How Dermatologists Diagnose Skin Infections
To diagnose a skin infection, we begin by asking questions to get more information about your rash. Typically, we want to learn about the rash’s onset, any potential triggers in your environment, your medical history, and any lifestyle factors.
Then, we’ll conduct a visual exam. This is a close examination of your skin, often using a dermascope. It’s not uncommon to perform a Wood’s Lamp exam as well—an inspection of the skin under UV light, which can make different microbes’ traits more visible and distinct.
Finally, a dermatologist will likely take a sample of the infection for analysis in a lab. Most often, the sample is a swab or skin scrape of the infected area. More rarely, we might take a skin biopsy (usually to rule out skin cancer, if there’s any ambiguity).
Once your dermatologist identifies the pathogen causing the infection, treatment can begin.
Types of Skin Infections
Skin infections differ by the type of infective pathogen, the symptoms they cause, and the skin tissues they impact. Pathogens may be bacteria, viruses, fungi, or parasites.
 Bacterial Skin Infections
Bacterial Skin Infections
The most common bacterial skin infections are:
- Impetigo, a shallow, blister-causing infection
- Cellulitis, an inflamed, painful infection of the dermis and subcutaneous fat
- Erysipelas, an infection of the epidermis causing a tender rash and fever
Staphylococcus aureus (staph), MRSA, Streptococcus pyogenes (group A strep)
Escherichia coli (E. coli), and Aeromonas hydrophila are frequent sources of these infections. Most can be treated without hospitalization. But, at their worst, they can cause necrotizing conditions, killing skin tissue entirely.
Viral Infections
Viruses can cause skin infections by targeting keratinocytes and other skin cells. The coxsackievirus causes hand-foot-and-mouth disease, spreading blisters and sores through the epidermis. Meanwhile, the molluscum contagiosum virus (MCV) and varicella-zoster virus (VZV) both cause raised, itchy red bumps.
Skin Parasites
Parasitic skin infections are the result of microbial insects, worms, or protozoa infesting skin tissue, often causing intense itching, inflammation, tenderness, or bleeding.
While some conditions, like the trematode-induced swimmer’s itch, end on their own, parasites better suited to human skin can cause serious, longer-term problems. Scabies, skin lice, cutaneous leishmaniasis, and larva-migrants-induced creeping eruption will continue or even worsen without treatment.
 Fungal Rashes
Fungal Rashes
The most commonplace fungal skin infections include ringworm, jock itch, candidiasis, Onychomycosis, Dermatophytosis, and versicolor. Depending on the type, pathogenic fungi can cause intense itching, skin discoloration, strange “cheese-like” residue, peeling or scaly skin, and even pus-filled cysts.
It’s easy to pass fungal infections onto others by contact, so early detection and swift treatment is key.
Treating Rashes & Skin Infections
Skin infection treatment varies depending on the infection’s underlying cause and its severity.
If the infecting pathogen is a virus, antivirals can be prescribed, but that’s not typical. Instead, most viral skin infections are treated with immune support and pain management.
Pharmaceutical Treatment
Most skin infections can be safely treated with pharmaceutical medications. Bacterial, fungal, parasitic, and viral infections demand distinct courses of treatment to be effective.
Cellulitis, Impetigo, Erysipelas (Bacterial Skin Infections)
Dermatologists treat most bacterial infections with oral antibiotics. Depending on the specific infecting pathogen, they usually prescribe penicillins, cephalosporins, tetracyclines, or certain sulfonamides. Limited, localized infections like impetigo can resolve with topical antibiotics, and the mildest cases may only need over-the-counter bacitracin creams.
In contrast, intravenous (IV) antibiotics are necessary when the infection is severe, or when it’s accompanied by systemic symptoms like fever or shortness of breath.
Candidiasis, Dermatophytosis, Versicolor & Ringworm (Fungal Skin Infections)
The majority of fungal skin infections are easier to treat topically than bacterial infections. Over-the-counter- and prescription-strength antifungals like miconazole, clotrimazole, terbinafine, or tioconazole, are effective as creams, topical powders, and shampoos.
Dermatologists prescribe oral antifungals when an infection persists or seems to worsen with topical treatment.
Lice, Scabies, Worms & Protozoa (Parasitic Skin Infections)
Infections caused by parasites like scabies, skin lice, or trematodes are treated with anthelmintics or antiprotozoals.
Certain non-prescription, topical antiparasitic creams can effectively treat most skin lice and scabies infections. Benzyl benzoate lotions, pyrethrins + piperonyl butoxide compounds, and permethrin creams are the most effective.
Other parasites, and persistent infections of skin lice or scabies, typically require highly potent, prescription-strength topical medications like thiabendazole, albendazole, ivermectin, or malathion.
Systematic treatment with an oral anti-parasitic (often miltefosine or ivermectin) is necessary to kill less-common parasitic skin infections, like cutaneous leishmaniasis or cutaneous filariasis. They’re also effective against severe cases of creeping eruption.
Surgical Intervention
Surgical Removal (Necrotizing Fasciitis & Skin Infection Complications)
Surgically removing infected or dead skin tissue is only an appropriate treatment for severe cases.
A dermatologist will most likely recommend surgical debridement—the removal of dead or infected tissue—when the infection causes thrombophlebitis, gangrene, or skin tissue necrosis. Debridement is often coupled with a skin graft or flap surgery, helping healthy skin regrow in the place where the infected skin once was.
Incision & Drainage (Pathogenic Abscess)
An abscess is a specific type of cyst: a bubble of pus in the skin, created by the immune system to contain and halt the spread of an infection. Typically, the pus is composed of the infecting microbe, dead skin cells, and white blood cells.
Abscesses are painful, red, inflamed, and can be entirely subdermal. They’re not uncommon complications of bacterial skin infections. More rarely, complex cases of VZV or dermatophytosis (i.e. cutaneous aspergillosis) create abscesses.
Draining any abscesses is an urgent priority when treating most skin infections.
Often, a dermatologist can drain an abscess in the office. It takes 20-60 minutes to complete the six-step process:
- Disinfect the skin
- Inject local anesthetics and epinephrine (to reduce bleeding)
- Cut the abscess
- Drain the pus using a syringe (or, if the cyst is large or deep, a catheter)
- Clean the drained abscess with a saline flush
- Dress and bandage the wound
The wound dressings are intended to allow for further, natural drainage if necessary, absorbing any new pus generated by the wound.
After the procedure is complete, dermatologists typically prescribe oral antibiotics and, if needed, antifungal medications.
Important
If you have an abscess that is growing in size, leaking pus, or is accompanied by systemic symptoms like fever, chills, or difficulty breathing, do not delay treatment. If you cannot get in to see a dermatologist that day, go to an Urgent Care center or the nearest emergency room.
Do not drain an abscess at home, as DIY drainage often spreads the infection.
Likewise, do not drain a kerion (a specific type of fungal abscess on the scalp, neck, or face). Unlike other types, kerions are best treated with systemic, oral antifungals, not incision.
Hair & Scalp Disorders
Hair and scalp disorders can cause uncomfortable or painful symptoms: intense itchiness, dandruff, follicle inflammation, and, for some, hair loss. Dermatologists are medical professionals who specialize in skin, scalp, hair, and nails.
We’re experts in the composition and function of the hair and scalp. They’re composed of diverse parts: keratin proteins, basket cells, sebum oil, epidermis tissue and melanocyte cells, just to name a few. A dermatologist can determine which parts are going wrong, and what treatments are most likely to set things right again.
Diagnosing & Treating Common Conditions
While many conditions can affect the hair and scalp, dermatologists most often see people dealing with one of the following problems.
 Alopecia Areata
Alopecia Areata
“Alopecia areata is a disease that happens when the immune system attacks hair follicles and causes hair loss. Hair follicles are the structures in skin that form hair…
…While hair can be lost from any part of the body, alopecia areata usually affects the head and face. Hair typically falls out in small, round patches about the size of a quarter, but in some cases, hair loss is more extensive. Most people with the disease are healthy and have no other symptoms.”
—NIH, Health Topics
Diagnosing Alopecia
To diagnose alopecia, a dermatologist typically uses a card to discern small hair breakage while visually inspecting the scalp for patterns of hair loss. Often, we’ll perform a “pull test,” gently tugging on about 40 strands of hair. If more than six hairs break or fall out in response to the gentle tug, it’s a sign of alopecia.
We will also swab the scalp to take a culture, and we may perform a small scalp biopsy. The swab culture can determine if an infection (like staph or ringworm) is causing the symptoms. The biopsy can be examined to rule out autoimmune conditions. It can also reveal the nature of any follicular damage, indicating which subtype of alopecia a person is dealing with.
Key Treatments
A dermatologist typically prescribes different treatments depending on the alopecia category and its underlying cause. These factors determine if the right treatment is a corticosteroid like triamcinolone acetonide, a vasodilator like minoxidil, or a JAK inhibitor like baricitinib (Olumiant®).
For some, light therapies are more effective than pharmaceuticals. In certain cases, psoralen ultraviolet light therapy (PUVA or PUVB) can effectively prevent the immune system’s attack on the scalp (and subsequent inflammation), while low-level laser light therapy (LLLT) can stimulate hair follicle growth.
Dandruff & Seborrheic Dermatitis
“Seborrheic Dermatitis (SD) and dandruff are of a continuous spectrum of the same disease that affects the seborrheic areas of the body[…] Seborrheic areas are those characterized by excessive oil production and inflammation of the skin[…].”
“Dandruff is restricted to the scalp, and involves itchy, flaking skin without visible inflammation. SD can affect the scalp as well as other seborrheic areas, and involves itchy and flaking or scaling skin, inflammation and pruritus [i.e. severe itching].”
—NIH Dictionary
Diagnosis & Treatment
A dermatologist can typically diagnose seborrheic dermatitis and dandruff by visual inspection.
It is rare to need a biopsy. The skin flakes and itchy scalp are often unambiguous signs. It can be caused by an overgrowth of Malassezia yeast (a fungus), excess sebum or keratin, or a dysfunction of the immune system.
Dermatologists usually prescribe anti-inflammatory steroids, sebum-control shampoos, and anti-fungal creams, lotions, and hair cleansers as treatment.
 Folliculitis
Folliculitis
Folliculitis is acne of the scalp. It’s caused by inflamed hair follicles, usually clogged with excess sebum, keratin, dead skin cells, bacteria, or fungus.
Diagnosing Folliculitis
To diagnose it, a dermatologist performs a visual inspection and asks questions about your medical history. We will often take a swab to determine the specific organism causing the problem.
On certain occasions, we’ll apply potassium hydroxide (KOH) to the scalp during the inspection, to make it easier to visualize hyphae and spores associated with fungal folliculitis.
Folliculitis Treatments
Treating folliculitis differs depending on whether it’s primarily caused by a bacterial infection or a fungus. Treating bacterial folliculitis requires antibiotics, typically topical antibiotics (clindamycin or mupirocin). If it resists topical treatment, we try oral antibiotics like cephalexin or dicloxacillin.
Fungal folliculitis is usually treated simultaneously with topical antifungals (shampoos) and oral antifungals. Antifungal shampoos with active ingredients like ketoconazole, miconazole, or zinc pyrithione, and supporting ingredients like selenium sulfide, salicylic acid, and ciclopirox, are most effective.
Steroid creams can also be prescribed to alleviate painful symptoms like inflammation and intense itchiness.
Folliculitis decalvans & PRP
One specific type of folliculitis, Folliculitis decalvans, can be treated with Platelet-rich plasma (PRP) therapy.
The growth factors and cytokines in a person’s blood platelets can reduce inflammation and stimulate hair growth. It’s an unusual treatment option, but it’s worth considering when folliculitis is moderate or severe.
Frequently Asked Questions
Medical dermatology and cosmetic dermatology are both specialized fields of medicine focused on skin, scalp, nails, and hair.
However, medical dermatology specifically centers on the diagnosis and treatment of skin disorders, infections, and other medical conditions primarily affecting those physical features. For example, a medical dermatologist may diagnose and treat eczema, ringworm, acne, or skin cancer.
In contrast, cosmetic dermatology centers on beauty and the aesthetics of skin. A cosmetic dermatologist might reduce the appearance of wrinkles or improve skin’s elasticity and glow.
Most adults should have a skin cancer screening once every year. However, people who face an elevated risk of skin cancer due to medical conditions or family history should screen for skin cancer 2-4 times per year.
Yes, our medical dermatology practice accepts most health insurance plans.
Please contact our office to verify your insurance plan’s eligibility. Or, call the number on your insurance card to verify that Clarus Dermatology is a covered provider.
Your first visit to a medical dermatologist centers on making sure the dermatologist has the information they need to effectively help you.
It typically involves answering thorough questions about your medical history, your current medications, your lifestyle, and any history of skin conditions in your family. The dermatologist will also listen and ask questions about all of your concerns, including any symptoms that led you to make the appointment.
An initial visit often includes a full-body skin exam. If you’re experiencing symptoms or the dermatologist notices something important, the second half of this visit will focus on potential diagnoses and identifying appropriate treatment options.
In many cases, the correct diagnosis is made and a treatment can be prescribed that same day.
Several factors affect how soon a psoriasis or eczema treatment achieves results, including:
- The condition’s severity
- The condition’s precise underlying cause in a given patient
- The type of treatment
Results vary based on the severity of the condition and the treatment used.
Yes. For lifestyle strategies, read our expert guides, “The Role of Diet In Maintaining Healthy Skin,” “Why Your Skincare Routine Isn’t Working” and, “How To Treat Psoriasis and Eczema In Cold Weather? 6 Tips From A Dermatologist.”
Of course, no two people have identical needs when it comes to clinical skin care. That’s why it’s so important to work with a dermatologist directly: it’s the best way to find an effective treatment tailored to your needs.